Primary Biliary Cholangitis (PBC) is a chronic liver disease that slowly damages the bile ducts inside your liver. These small ducts carry bile, a fluid that helps digest fats and remove waste from the body. When the bile ducts are damaged, bile builds up in the liver, leading to inflammation, scarring, and eventually liver damage.
PBC affects thousands of people in the United States, especially women between the ages of 30 and 60. Although it cannot always be completely cured, early diagnosis and proper treatment can help slow the disease’s progression and improve quality of life.
This article explains how PBC is diagnosed and treated, and what you can do to protect your liver health.
Understanding Primary Biliary Cholangitis (PBC)
PBC is considered an autoimmune disease. This means that your immune system, which normally protects you from infections, mistakenly attacks healthy cells in your liver’s bile ducts. Over time, this causes inflammation and scarring (fibrosis) that can eventually lead to cirrhosis, or severe liver damage.
While the exact cause of PBC is not known, doctors believe genetics, environmental triggers, and immune system dysfunction all play a role.
Common Symptoms of PBC
PBC develops slowly, and symptoms can vary from person to person. Many people may not notice symptoms in the early stages. As the disease progresses, you might experience:
- Fatigue (extreme tiredness)
- Itchy skin (pruritus)
- Dry eyes and mouth
- Abdominal pain (especially in the upper right side)
- Yellowing of the skin or eyes (jaundice)
- Swelling in the legs or abdomen
- Dark urine or pale stools
Because PBC can be silent for years, routine liver function tests and early check-ups play a vital role in identifying it before major damage occurs.
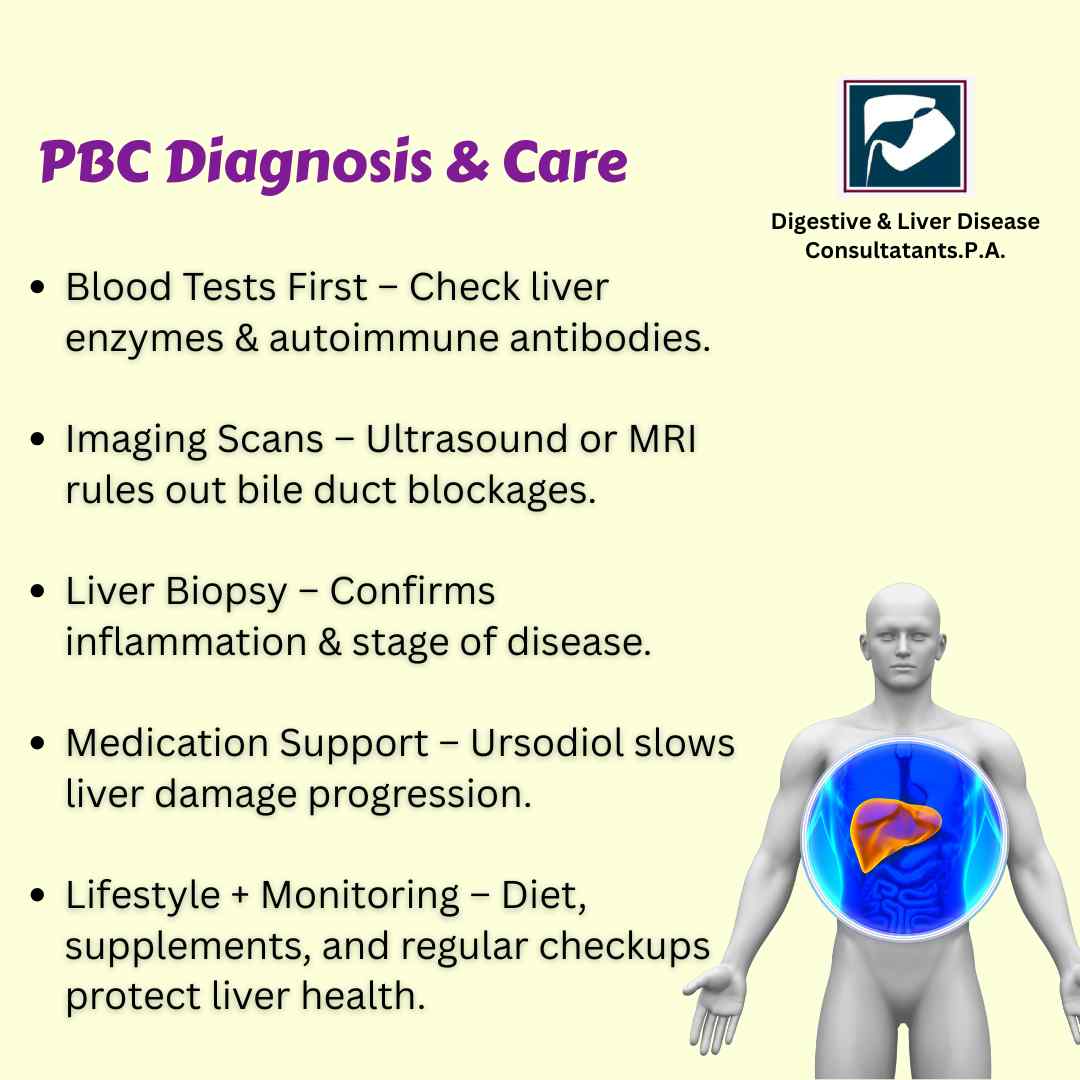
How Is PBC Diagnosed?
Diagnosing Primary Biliary Cholangitis requires a combination of medical history review, physical exams, and diagnostic tests. A gastroenterologist or hepatologist (liver specialist) will evaluate symptoms and recommend specific investigations.
1. Blood Tests
Blood tests are often the first step in diagnosis. They help assess liver function and detect the presence of antibodies linked to PBC. Key tests include:
- Liver Function Tests (LFTs): These measure enzymes like alkaline phosphatase (ALP), which is often elevated in PBC.
- Antimitochondrial Antibody (AMA) Test: A positive AMA test strongly suggests PBC, as this antibody is found in about 95% of cases.
- Other Autoantibodies: Additional tests may include ANA (antinuclear antibody) or anti-gp210, which support the diagnosis.
2. Imaging Tests
Imaging helps doctors see the structure of the liver and bile ducts.
- Ultrasound: A non-invasive test that checks for blockages or abnormalities in the liver and bile ducts.
- MRCP (Magnetic Resonance Cholangiopancreatography): A specialized MRI scan that provides detailed images of the bile ducts without using invasive procedures.
3. Liver Biopsy
In some cases, a liver biopsy may be done. A small sample of liver tissue is taken and examined under a microscope to confirm inflammation, scarring, or other changes typical of PBC.
These tests not only confirm the diagnosis but also help doctors determine how far the disease has progressed.
How Is PBC Treated?
While there is no complete cure for Primary Biliary Cholangitis, treatments can slow its progression, relieve symptoms, and prevent complications. The main goals of treatment are to protect the liver, improve bile flow, and maintain overall health.
1. Medications to Improve Bile Flow
Ursodeoxycholic Acid (UDCA): This is the first-line treatment for PBC. UDCA helps improve bile flow and reduce liver damage. Many people respond well to this medication, especially when started early.
Obeticholic Acid (OCA): If UDCA is not effective or not well tolerated, your doctor may prescribe OCA. This drug helps regulate bile acid production and reduce inflammation.
2. Managing Symptoms
Itching: Medications like cholestyramine, rifampicin, or antihistamines may help relieve severe itching.
Fatigue: While fatigue can be difficult to treat, maintaining a healthy sleep routine and managing stress may help.
Dry Eyes and Mouth: Artificial tears or saliva substitutes can provide relief.
3. Preventing Complications
PBC can lead to vitamin deficiencies because bile is needed to absorb fat-soluble vitamins (A, D, E, and K). Your doctor may recommend supplements to prevent these deficiencies.
Bone health can also be affected, leading to osteoporosis. Calcium and vitamin D supplements, along with weight-bearing exercises, are often advised.
If PBC progresses to cirrhosis or liver failure, a liver transplant may be necessary. With proper care, many people with PBC live full, active lives for decades before advanced treatment is needed.
Lifestyle and Self-Care Tips for PBC
- Eat a balanced diet: Choose foods rich in fiber, lean proteins, and healthy fats. Avoid high-fat, fried, and processed foods.
- Limit alcohol: Alcohol can worsen liver damage, so it’s best to avoid it completely.
- Stay hydrated: Water supports healthy digestion and liver function.
- Exercise regularly: Gentle physical activity like walking or yoga can improve energy and strengthen bones.
- Avoid unnecessary medications: Always consult your doctor before taking supplements or over-the-counter medicines that may affect your liver.
About Digestive & Liver Disease Consultants, P.A.
At Digestive & Liver Disease Consultants, P.A., our team of board-certified gastroenterologists specializes in diagnosing and treating a wide range of digestive and liver conditions, including Primary Biliary Cholangitis (PBC). Using advanced diagnostic tools and evidence-based treatments, we provide personalized care tailored to each patient’s needs.
We focus on early detection and long-term management of liver diseases to help patients live healthier lives. Whether you need a routine liver check-up, advanced imaging, or ongoing treatment for chronic liver conditions, our team is here to guide you every step of the way.
Conclusion
Primary Biliary Cholangitis can be a serious condition, but with early diagnosis, proper medical treatment, and lifestyle care, many people manage it successfully. Regular check-ups and working closely with your gastroenterologist are key to preventing complications and maintaining liver health.
If you experience persistent fatigue, itching, or abnormal liver test results, don’t wait. Schedule a consultation with Digestive & Liver Disease Consultants, P.A. Our expert gastroenterologists can help diagnose PBC early and create a treatment plan that protects your liver and improves your quality of life.