Inflammatory Bowel Disease, commonly known as IBD, is a chronic condition that causes inflammation of the digestive tract. Because its symptoms often overlap with other digestive disorders, reaching an accurate diagnosis requires careful evaluation. Many patients spend months or even years experiencing symptoms before receiving clarity. Understanding the IBD diagnostic process helps patients know what to expect and why multiple tests are often needed.
Early and accurate IBD diagnosis is critical. It allows timely treatment, prevents complications, and improves long term quality of life.
Understanding Inflammatory Bowel Disease
IBD mainly includes two conditions: Crohn’s disease and ulcerative colitis. Both involve chronic inflammation, but they affect different parts of the digestive tract and behave differently.
Crohn’s disease can affect any part of the digestive system from mouth to anus, while ulcerative colitis affects only the colon and rectum. Because of these differences, Crohn’s disease diagnosis and ulcerative colitis diagnosis follow similar but not identical paths.
Symptoms Leading to IBD Diagnosis
The diagnostic journey usually begins when symptoms persist or worsen over time. Common symptoms leading to IBD diagnosis include
- Chronic diarrhea
- Blood or mucus in stool
- Abdominal pain or cramping
- Urgency to pass stool
- Fatigue
- Unexplained weight loss
- Anemia
These symptoms are not exclusive to IBD, which is why further testing is essential.
Differentiating IBS and IBD
One of the most important steps in the IBD diagnostic process is differentiating IBS and IBD. Irritable Bowel Syndrome is a functional disorder, while IBD causes visible inflammation and tissue damage.
Key differences include:
- IBS does not cause bleeding or inflammation
- IBD can lead to anemia and weight loss
- IBS does not damage the intestines
- IBD requires objective testing for confirmation
Because symptoms may appear similar, laboratory and imaging studies play a crucial role.
Initial Medical Evaluation
How doctors diagnose IBD starts with a detailed medical history and physical examination. A gastroenterologist will assess
• Symptom duration and severity
• Family history of IBD or autoimmune disease
• Previous infections or antibiotic use
• Dietary triggers and stress patterns
This information helps guide the choice of inflammatory bowel disease tests.
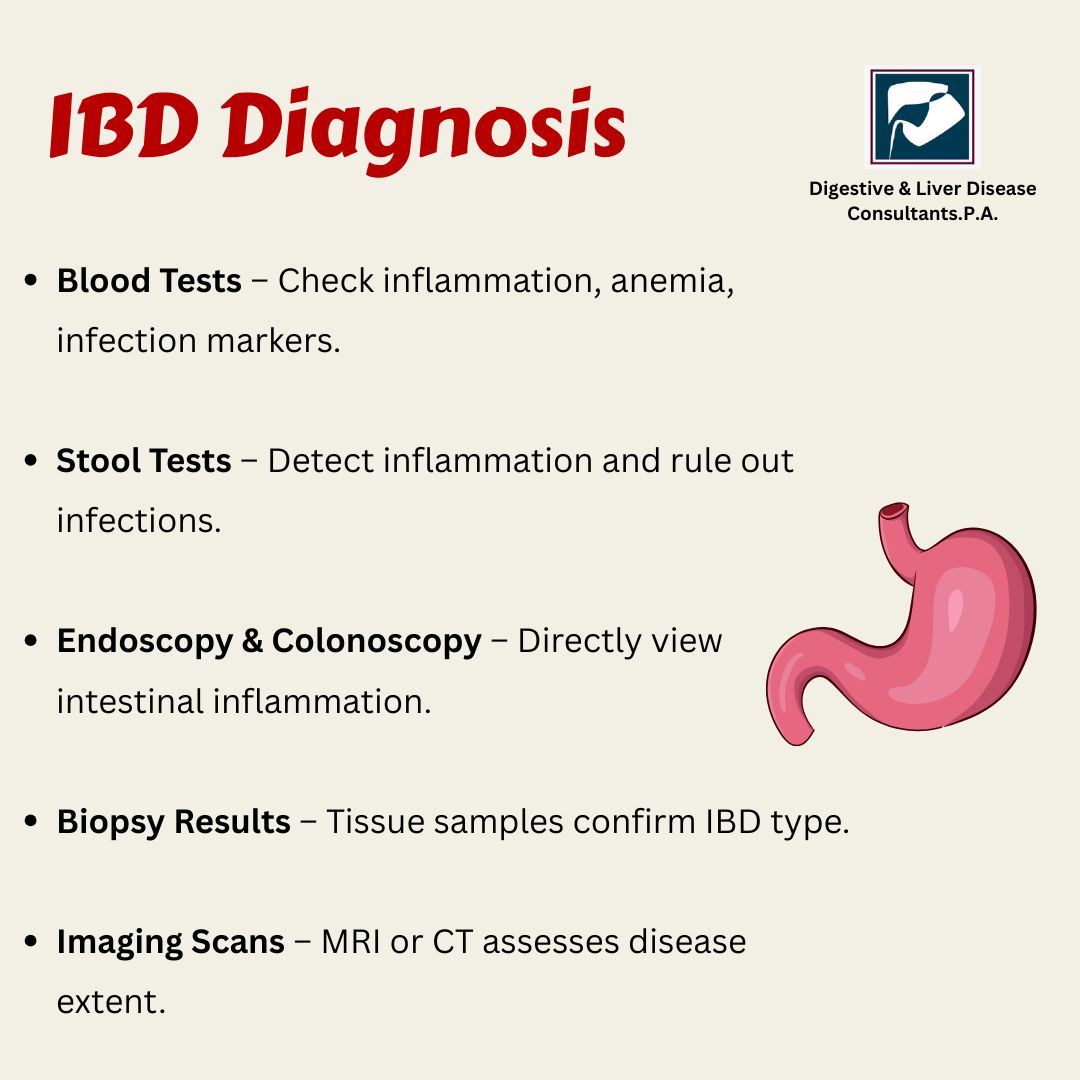
IBD Blood Tests
IBD blood tests are often the first step in evaluation. While they cannot confirm IBD on their own, they provide important clues.
Common blood tests include:
- Complete blood count to check for anemia
- Inflammatory markers such as CRP and ESR
- Electrolyte and nutritional status tests
Elevated inflammation markers support the possibility of active disease but are not specific to IBD.
Stool Tests for IBD
Stool tests for IBD help rule out infections and assess intestinal inflammation.
These tests may include
- Fecal calprotectin to detect intestinal inflammation
- Stool cultures to rule out bacterial or parasitic infections
- Tests for blood in stool
Fecal calprotectin is particularly useful in IBD screening methods and in distinguishing IBD from IBS.
Colonoscopy for IBD
Colonoscopy for IBD is the most important diagnostic tool. It allows direct visualization of the colon and terminal ileum and helps confirm inflammation.
During a colonoscopy, the gastroenterologist can
- Identify areas of inflammation or ulcers
- Determine disease extent and severity
- Take biopsies for microscopic examination
Biopsy results help confirm the diagnosis and differentiate Crohn’s disease from ulcerative colitis.
Endoscopic Findings and Biopsy Results
Biopsies taken during colonoscopy reveal characteristic tissue changes. These findings are essential for confirming IBD diagnosis.
Biopsy analysis helps
- Confirm chronic inflammation
- Identify disease pattern
- Rule out infections or cancer
- Support Crohn’s disease diagnosis or ulcerative colitis diagnosis
No single test is enough. Diagnosis relies on combined findings.
Imaging Tests for IBD
Imaging tests for IBD are used to evaluate parts of the digestive tract that cannot be seen during colonoscopy.
Common imaging tests include
- CT enterography
- MRI enterography
- Ultrasound in select cases
These tests are especially useful for detecting complications such as strictures, fistulas, or deep inflammation in Crohn’s disease.
Upper Endoscopy in Selected Cases
If symptoms suggest upper digestive tract involvement, an upper endoscopy may be recommended. This is more common in Crohn’s disease diagnosis.
It allows evaluation of the esophagus, stomach, and upper small intestine.
IBD Screening Methods and Risk Assessment
There is no single screening test for IBD in the general population. However, IBD screening methods are used for individuals with persistent symptoms or family history.
Screening focuses on
- Symptom assessment
- Inflammatory markers
- Stool testing
- Endoscopic evaluation when indicated
Early diagnosis of IBD improves treatment response and reduces complications.
Why Early Diagnosis of IBD Matters?
Delaying diagnosis can lead to disease progression and complications such as
- Severe inflammation
- Intestinal narrowing or obstruction
- Malnutrition
- Increased cancer risk
- Reduced quality of life
Early diagnosis of IBD allows timely treatment and better long term outcomes.
The Role of a Gastroenterologist in IBD Diagnosis
A gastroenterologist IBD diagnosis is essential because IBD requires specialized expertise. Interpreting test results, biopsy findings, and imaging studies requires experience.
A gastroenterologist ensures
- Accurate diagnosis
- Differentiation between Crohn’s disease and ulcerative colitis
- Appropriate treatment planning
- Ongoing disease monitoring
The Complete IBD Diagnostic Process
The IBD diagnostic process is step by step and may take time. It typically includes
- Symptom evaluation
- Blood and stool tests
- Colonoscopy with biopsy
- Imaging studies when needed
- Ongoing follow up and reassessment
This comprehensive approach ensures accuracy and safety.
Why Choose Digestive & Liver Disease Consultants, P.A.?
Diagnosing IBD requires precision, experience, and advanced diagnostic tools. Digestive & Liver Disease Consultants, P.A. offers comprehensive evaluation for patients with suspected inflammatory bowel disease.
What patients can expect
- Board certified gastroenterologists
- Advanced endoscopic and imaging facilities
- Complete inflammatory bowel disease testing
- Personalized diagnostic and treatment planning
- Focus on early and accurate diagnosis
Our team prioritizes clarity, early intervention, and long term digestive health.
Conclusion
IBD diagnosis is not based on symptoms alone. It requires a careful combination of blood tests, stool tests, colonoscopy, imaging studies, and expert evaluation. Understanding how doctors diagnose IBD helps patients feel informed and confident during the process.
Early diagnosis allows better disease control, fewer complications, and improved quality of life. If symptoms persist, professional evaluation is essential.
If you are experiencing ongoing digestive symptoms or suspect inflammatory bowel disease, consult our top gastro specialist at Digestive & Liver Disease Consultants, P.A. Accurate diagnosis is the first step toward effective treatment and long term relief. Schedule your consultation today and take control of your digestive health.