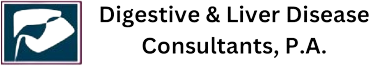
Hemorrhoids are one of the most common digestive issues people face but often the least talked about. They can cause discomfort, pain, itching, and bleeding, yet many people hesitate to seek medical help due to embarrassment. One common question is — do hemorrhoids heal without treatment?
The answer depends on several factors, including the type, severity, and lifestyle habits of the individual. Some mild hemorrhoids can improve on their own, while others may require medical care to prevent complications. Let’s understand this condition in detail and when it’s time to see a gastroenterologist.
What Are Hemorrhoids?
Hemorrhoids, also known as piles, are swollen veins in the lower rectum or anus. They can develop inside the rectum (internal hemorrhoids) or under the skin around the anus (external hemorrhoids). These veins become enlarged when there is increased pressure in the lower rectum — often due to straining during bowel movements, chronic constipation, or prolonged sitting.
Common Causes Include:
- Straining during bowel movements
- Sitting for long periods, especially on the toilet
- Chronic constipation or diarrhea
- Obesity
- Pregnancy
- Low-fiber diet
- Aging and weakened rectal tissues
Can Hemorrhoids Heal on Their Own?
In some cases, yes. Mild hemorrhoids, especially those caused by temporary factors like constipation or pregnancy, can shrink and heal on their own with simple lifestyle changes. The body can naturally reduce inflammation, and symptoms like pain and bleeding may fade within a few days.
However, moderate to severe hemorrhoids often persist or worsen over time if not properly managed. Ignoring symptoms can lead to complications such as persistent bleeding, blood clots (thrombosed hemorrhoids), or anemia due to chronic blood loss.
Signs That Hemorrhoids Are Healing
If your hemorrhoids are improving naturally, you may notice:
- Reduced swelling or discomfort
- Less itching or irritation
- Decrease in bleeding during bowel movements
- Easier and softer stools due to better diet and hydration
Healing can take anywhere from a few days to a few weeks, depending on the severity and care taken during recovery.
When Hemorrhoids Won’t Heal on Their Own
Sometimes, home care isn’t enough. Hemorrhoids that are large, painful, or frequently bleeding usually require medical attention.
You should see a gastroenterologist if you experience:
- Rectal bleeding that doesn’t stop
- Severe pain or swelling near the anus
- A hard lump that feels tender (possible thrombosed hemorrhoid)
- Mucus discharge or a feeling of incomplete bowel movement
- Bleeding that continues after a few weeks of home care
Persistent symptoms may also be a sign of another digestive condition, such as anal fissures, polyps, or colorectal cancer. Getting a proper diagnosis ensures you receive the right treatment.
Home Remedies and Lifestyle Changes for Relief
For mild hemorrhoids, simple at-home steps can help reduce pain and speed up healing.
1. Increase Fiber Intake
A fiber-rich diet softens stool and reduces strain during bowel movements. Eat plenty of fruits, vegetables, whole grains, and legumes. Fiber supplements like psyllium (Metamucil) can also help.
2. Stay Hydrated
Drinking enough water throughout the day helps prevent constipation, which is a major cause of hemorrhoids.
3. Use Warm Sitz Baths
Soaking the anal area in warm water for 10–15 minutes a few times a day can relieve itching, swelling, and discomfort.
4. Avoid Straining and Prolonged Sitting
Try not to sit on the toilet for long periods. Straining increases pressure in the veins, making hemorrhoids worse.
5. Apply Over-the-Counter Creams or Wipes
Hemorrhoid creams or medicated wipes containing witch hazel or hydrocortisone can provide temporary relief from pain and itching.
6. Exercise Regularly
Gentle activities like walking improve circulation, prevent constipation, and reduce pressure on rectal veins.
Medical Treatments for Persistent Hemorrhoids
If symptoms do not improve within a few weeks, your doctor may recommend non-surgical or surgical treatments depending on the severity.
Non-Surgical Options
- Rubber band ligation: A small band is placed around the base of the hemorrhoid to cut off blood flow, causing it to shrink.
- Sclerotherapy: A chemical solution is injected to shrink the hemorrhoid.
- Infrared coagulation: Heat is used to seal the hemorrhoid tissue.
Surgical Options
Hemorrhoidectomy: Surgical removal of large or severe hemorrhoids.
Stapled hemorrhoidopexy: Used for internal hemorrhoids that have prolapsed (bulged out).
Your gastroenterologist will recommend the best option based on your symptoms and overall health.
Preventing Hemorrhoids from Returning
Even after healing, hemorrhoids can return if lifestyle habits don’t change. To prevent recurrence:
- Eat a balanced, high-fiber diet
- Stay well hydrated
- Maintain a healthy body weight
- Exercise regularly
- Avoid straining during bowel movements
- Respond promptly to the urge to pass stool
These habits support overall digestive health and reduce the risk of other GI conditions as well.
About Digestive & Liver Disease Consultants, P.A.
At Digestive & Liver Disease Consultants, P.A., our board-certified gastroenterologists provide expert care for all types of digestive and liver conditions, including hemorrhoids, constipation, rectal bleeding, and inflammatory bowel disease. With state-of-the-art diagnostic tools and compassionate, patient-centered care, our team helps you find lasting relief and improve your quality of life.
We serve patients across Texas with personalized treatment plans designed for effective, long-term digestive wellness.
Conclusion
So, do hemorrhoids heal without treatment? In many mild cases, yes — simple diet changes, hydration, and proper hygiene can help your body recover naturally. But if your symptoms are severe, frequent, or not improving, professional medical care is essential.
Early diagnosis and expert treatment can prevent complications and help you return to normal life comfortably.
If you’re experiencing pain, bleeding, or discomfort from hemorrhoids, schedule a consultation with Digestive & Liver Disease Consultants, P.A. Our experienced gastroenterologists can provide relief and help you restore healthy digestion.